Understanding the science behind how bottling up your emotions can damage your immune system
We’ve all heard the advice: “Just be positive!” or “Don’t let it get to you.”
But what if the very act of suppressing negative emotions, from grief and anger to stress and anxiety, does more than just affect your mood? What if it actually makes you sick?
The emerging field of psychoneuroimmunology (PNI) reveals a startling truth: your emotional landscape directly shapes your physical health through intricate brain-immune system connections.
Suppressing emotions isn’t just a psychological issue; it’s a full-body physiological event that can dysregulate your immune system, trigger chronic inflammation, and increase your risk for serious illnesses.
What Is Psychoneuroimmunology?
Psychoneuroimmunology studies how psychological processes interact with the nervous and immune systems to influence overall health. This interdisciplinary field has exploded over the past three decades, revealing that our thoughts, feelings, and behaviors aren’t isolated in our heads; they trigger cascades of biological responses throughout our entire bodies.
At its core, PNI operates on a simple principle: your brain and immune system are in constant, bidirectional communication. When you experience emotions, your brain activates neural and endocrine pathways that directly influence immune cell function. Conversely, immune signals (like cytokines) feed back to your brain, affecting your mood, cognition, and behavior.
The Emotional Suppression-Stress-Immune Pathway
Emotional Suppression & Immune System: How It Triggers Stress Responses
Emotional suppression is a conscious effort to inhibit the expression of felt emotions. While it might seem like a useful short-term strategy, research shows it activates the body’s stress machinery in powerful ways. A meta-analysis of 24 studies found that experimentally manipulated emotion suppression was associated with greater physiological stress reactivity, particularly in cardiac, hemodynamic, and neuroendocrine parameters.
When you suppress emotions, your body remains in a state of heightened stress. Your sympathetic nervous system stays activated, continuously releasing stress hormones like cortisol and norepinephrine. Unlike healthy emotional processing, which allows the stress response to resolve, suppression keeps you locked in a physiological “fight-or-flight” state.
The HPA Axis: Your Body’s Stress Command Center
The key player in this process is the hypothalamic-pituitary-adrenal (HPA) axis. Here’s how it works:
- Emotional stressor → activates the hypothalamus
- Hypothalamus releases CRH (corticotropin-releasing hormone)
- CRH triggers the pituitary to release ACTH (adrenocorticotropic hormone)
- ACTH stimulates the adrenal glands to produce cortisol (the primary stress hormone)
In healthy situations, cortisol provides negative feedback to shut down this system. But chronic emotional suppression disrupts this feedback loop, leading to sustained hypercortisolism and glucocorticoid resistance, where anti-inflammatory effects become impaired and pro-inflammatory processes go unchecked.

Cytokines: The Molecular Messengers of Sickness
What Are Cytokines?
Cytokines are small proteins released by immune cells that act as messengers, coordinating immune responses. In the context of emotional suppression, several key cytokines become dysregulated:
- Interleukin-6 (IL-6): A primary driver of inflammation, consistently elevated in depression and chronic stress
- Interleukin-1β (IL-1β): Promotes inflammatory responses and is linked to post-infarction depression
- TNF-α (Tumor Necrosis Factor-alpha): Another pro-inflammatory cytokine elevated in depression and PTSD

The Inflammation-Depression Connection
Meta-analyses show strong associations between depression and inflammatory markers. People with depression show elevated levels of IL-6, IL-1, TNF-α, and C-reactive protein (CRP) → a key marker of systemic inflammation.
Critically, this isn’t just correlation. Longitudinal studies demonstrate that inflammation predicts the development of depression, and experimentally inducing inflammation (with vaccines or interferon treatment) can produce depressive symptoms in previously healthy individuals, suggesting inflammation is a causal pathway, not merely a consequence.
Why This Makes You Physically Sick
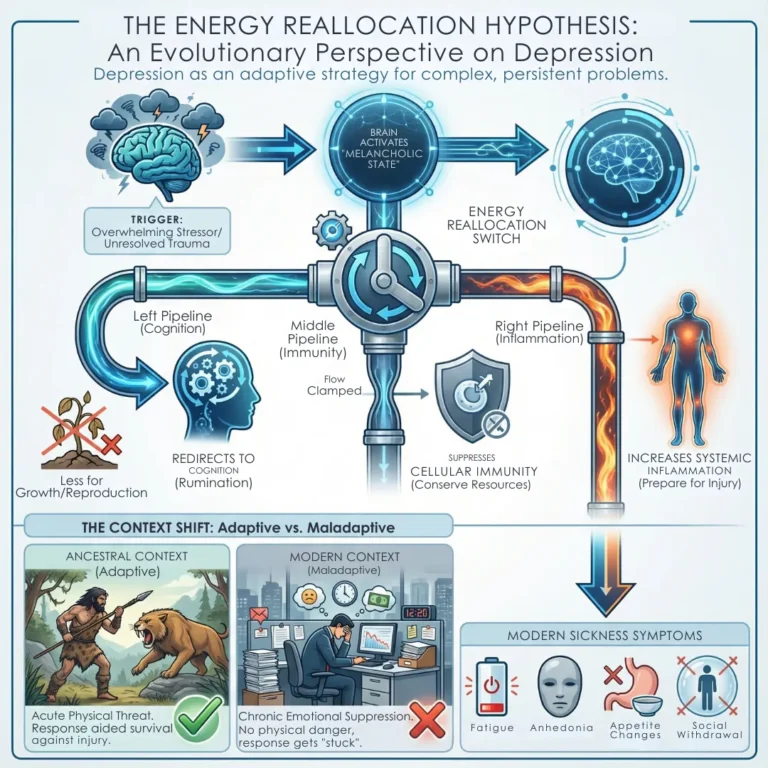
The Energy Reallocation Hypothesis
Recent evolutionary perspectives suggest that depression could be an adaptive energy reallocation strategy triggered by complex, persistent problems. When your brain detects an overwhelming stressor (like unresolved emotional trauma), it activates a “melancholic” state that:
- Redirects energy from growth and reproduction to cognition (rumination)
- Suppresses cellular immunity to conserve resources
- Increases systemic inflammation to prepare for potential injury
While this might have been adaptive for our ancestors facing physical threats, in modern life—with chronic emotional suppression rather than acute physical danger—it becomes maladaptive, leading to sickness symtoms such as fatigue, anhedonia, appetite changes, and social withdrawal.
Physical Health Consequences
The downstream effects of the emotional suppression immune system interaction are profound.
Distress-related immune dysregulation has been linked to:
Cardiovascular disease:
- Chronic inflammation damages blood vessels and promotes atherosclerosis
- Gastrointestinal disorders: Stress alters gut permeability and microbiome composition
- Autoimmune diseases: Dysregulated cytokine patterns can trigger or worsen conditions like lupus and rheumatoid arthritis
- Metabolic syndrome: Inflammation contributes to insulin resistance and type 2 diabetes
- Accelerated aging: Chronic inflammation is a hallmark of aging-related decline
- Impaired wound healing: Suppressed immune function delays recovery from injury
The Biological Mechanism: A Three-System Loop
The Neural Pathway
Emotional suppression activates brain regions involved in conflict monitoring and self-control. This sustained cognitive effort drains executive function and activates stress circuits, particularly the amygdala (fear centre) and medial prefrontal cortex.
The Endocrine Pathway
As described above, HPA activation leads to chronic cortisol exposure. Paradoxically, while cortisol is anti-inflammatory acutely, chronic exposure causes glucocorticoid resistance, where cells become less responsive and inflammation increases.
The Immune Pathway
Elevated cortisol and sympathetic activation stimulate immune cells to release pro-inflammatory cytokines. These cytokines then:
- Signal back to the brain to induce “sickness behavior” (fatigue, anhedonia, social withdrawal)
- Disrupt neurotransmitter metabolism, particularly serotonin and dopamine systems
- Alter synaptic plasticity in brain regions controlling mood and cognition
This creates a vicious cycle: emotional suppression → chronic stress → inflammation → depressive symptoms → more emotional suppression.

Breaking the Cycle: What the Research Shows
Why Suppression Is Different From Processing
It’s crucial to understand that not all negative emotions are harmful. The problem is suppression, not feeling. Studies show:
- Emotional disclosure and processing activate different neural pathways than suppression and are associated with better immune outcomes
- Expressive writing about traumatic experiences can reduce physician visits and improve immune markers
- Mindfulness-based interventions that teach acceptance rather than suppression can reduce inflammatory markers
The Antidote: Adaptive Processing
Evolutionary models suggest that rumination (persistent, analytical thinking about problems) can be adaptive when it leads to root cause analysis and problem-solving. The key is moving from passive suppression to active processing:
- Identify triggers: What emotions are you suppressing?
- Acknowledge without judgment: Allow yourself to feel without immediate reaction
- Analyze constructively: Use Type 2 processing (deliberate, analytical thinking) to understand causes and solutions
- Take action: Implement changes based on insights
- Seek support: Social connection reduces inflammation and buffers stress
Practical Takeaways: Protecting Your Health
- Recognize Emotional Suppression
- Common signs include:
- Forcing a smile when you’re upset
- Changing the subject when emotions arise
- Saying “I’m fine” when you’re not
- Using substances or distractions to avoid feelings
- Common signs include:
- Build Emotional Awareness
- Wearable devices can now track physiological markers (HRV, sleep, activity) that indicate emotional suppression patterns. These provide objective feedback on when your stress systems are activated
- Practice Healthy Emotional Processing
- Instead of suppressing:
- Journaling: Writing about emotions reduces HPA activation
- Therapeutic interventions: Acceptance and Commitment Therapy (ACT), Cognitive Behavioral Therapy (CBT), and exposure-based therapies have been shown to reduce inflammatory markers
- Social connection: Close relationships diminish negative emotions and enhance immune regulation 3
- Instead of suppressing:
- Monitor Your Physical Markers
- If you’re experiencing:
- Unexplained fatigue
- Frequent infections
- Slow wound healing
- Gastrointestinal issues
- Chronic inflammation markers
- If you’re experiencing:
These may be signs that emotional suppression is impacting your immune system.
Listen to Your Body’s Signals
Psychoneuroimmunology teaches us a profound lesson: emotional suppression isn’t a sign of strength; it’s a physiological stressor that can make you physically sick. The evidence is overwhelming: when you chronically suppress emotions, you activate stress pathways, trigger inflammatory cascades, and dysregulate the delicate balance between your brain and immune system.
The good news? The same research that reveals this connection also points to solutions. Processing emotions rather than suppressing them, seeking social support, and using evidence-based psychological interventions can reverse these harmful patterns and restore immune balance.
Your emotions aren’t just “in your head”, they’re in every cell of your body. Learning to process them healthily isn’t just psychological self-care; it’s whole-body healthcare.
Further Reading
- Emotional suppression: Physiology, self-report, and expressive behavior.
- Composure at Any Cost? The Cognitive Consequences of Emotion Suppression
- Is Emotional Suppression Always Bad? A Matter of Flexibility and Gender Differences
- Culture, emotion suppression and disclosure, and health
- The Neural Bases of Emotion Regulation: Reappraisal and Suppression of Negative Emotion
Disclaimer:
This information is for educational purposes only and does not constitute professional medical advice. Always consult a healthcare professional before incorporating any new therapy into your practice.
Do you want to see all the updates?
👉 Follow us on Instagram and Facebook and never miss a thing!